Imagine a patient lying in bed, their skin pale and dry, their lips cracked, and their eyes sunken. Their voice is weak, barely a whisper, and their heart beats rapidly. This is the reality of a patient experiencing a fluid volume deficit, a condition that can quickly become life-threatening without proper intervention. As a nurse, I’ve witnessed firsthand the urgency and importance of a comprehensive nursing care plan for these patients. This article will delve into fluid volume deficit, its causes, symptoms, and the critical role of nurses in providing safe and effective care.
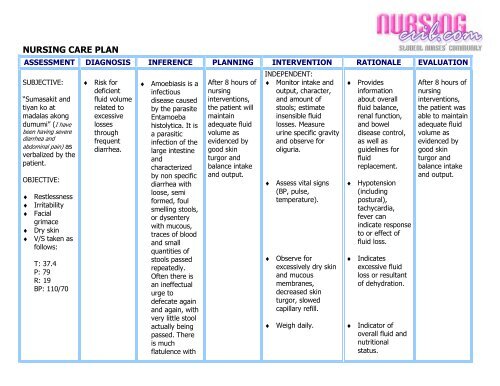
Image: slidesharetrick.blogspot.com
Fluid volume deficit, also known as dehydration, is a serious medical condition that occurs when the body loses more fluids than it takes in. This imbalance can disrupt essential physiological processes, leading to complications that range from mild discomfort to organ failure. Understanding the nuances of fluid volume deficit and implementing a tailored nursing care plan can make a significant difference in patient outcomes.
Understanding Fluid Volume Deficit
Defining Fluid Volume Deficit
Fluid volume deficit, or dehydration, is a condition where the body loses more fluids than it takes in. This results in a decrease in the total body water content, affecting various bodily functions, particularly blood volume and circulation.
Causes of Fluid Volume Deficit
Fluid volume deficit can arise from various causes, including:
- Inadequate fluid intake: This can occur due to lack of access to water, difficulty swallowing, or simply forgetting to drink.
- Excessive fluid loss: This can be due to factors such as:
- Gastrointestinal losses: Vomiting, diarrhea, and nasogastric suctioning.
- Renal losses: Diuretic use or kidney disease.
- Skin losses: Excessive sweating, burns, open wounds.
- Respiratory losses: Rapid breathing or prolonged coughing.
- Third-space fluid shifts: This occurs when fluid moves from the vascular space to interstitial spaces, like in cases of burns or trauma.
Image: nurseslabs.com
Symptoms of Fluid Volume Deficit
The symptoms of fluid volume deficit can vary depending on the severity of dehydration. Mild dehydration may manifest with:
- Thirst
- Dry mouth
- Fatigue
- Headache
- Dizziness
- Decreased urine output
- Constipation
Severe dehydration can lead to more serious symptoms, such as:
- Rapid heart rate
- Low blood pressure
- Sunken eyes
- Decreased skin turgor (skin elasticity)
- Confusion
- Seizures
- Coma
Nursing Assessment and Interventions
As nurses, our primary role in managing fluid volume deficit is to assess the patient’s condition accurately and promptly intervene to restore fluid balance. Here’s a breakdown of essential nursing interventions:
- Assessment: A thorough assessment is crucial to identify the cause and severity of fluid volume deficit. This includes taking vital signs (temperature, pulse, respiration, blood pressure), monitoring urine output, assessing skin turgor, and evaluating the patient’s mental status.
- Fluid Replacement: The primary intervention for fluid volume deficit is fluid replacement. This can be achieved through:
- Oral rehydration: Encourage the patient to drink fluids like water, electrolyte solutions, or broths, as tolerated.
- Intravenous (IV) fluid therapy: When oral rehydration is not possible or inadequate, IV fluids are administered to quickly replenish lost fluids and electrolytes.
- Electrolyte Monitoring: Dehydration can lead to electrolyte imbalances, so it’s essential to monitor serum electrolytes (sodium, potassium, chloride, etc.) regularly and correct any abnormalities.
- Medication Administration: Depending on the cause of fluid volume deficit, the nurse may administer medications like antiemetics (for vomiting), antidiarrheals, or diuretics (in case of fluid overload).
- Patient Education: It’s crucial to educate patients and their families about the cause of fluid volume deficit, its potential complications, and preventive measures.
Fluid Volume Deficit Nursing Care Plan: A Detailed Approach
A comprehensive nursing care plan for fluid volume deficit should include the following components:
Assessment
The initial assessment is crucial for establishing a baseline and guiding the nursing care plan.
- Vital Signs: Monitor temperature, pulse, respiration, blood pressure, and oxygen saturation frequently, as dehydration can impact cardiovascular function and oxygenation.
- Hydration Status: Assess skin turgor, mucous membranes, and urine output to gauge the severity of fluid volume deficit.
- Electrolyte Levels: Obtain laboratory tests to monitor electrolyte levels and identify potential imbalances, particularly sodium, potassium, and chloride.
- Fluid Intake and Output: Accurately record all fluid intake (oral, IV fluids) and output (urine, vomit, drainage) to ensure appropriate fluid balance.
- Mental Status: Assess for confusion, lethargy, or other changes in mental status, as these can indicate severe dehydration and impending complications.
Nursing Diagnoses
Based on the assessment findings, the nurse will formulate nursing diagnoses that guide the development of specific interventions. Common nursing diagnoses for fluid volume deficit include:
- Fluid Volume Deficit: This diagnosis reflects the actual physiological condition of fluid depletion.
- Risk for Dehydration: This diagnosis applies to patients who are at risk of developing fluid volume deficit due to factors like vomiting, diarrhea, or excessive sweating.
- Ineffective Tissue Perfusion: This diagnosis reflects the potential for decreased tissue oxygenation due to impaired circulation resulting from fluid volume deficit.
- Acute Confusion: Dehydration can affect brain function, leading to confusion, disorientation, and altered mental status.
Nursing Interventions
Once nursing diagnoses are established, the nurse will implement specific interventions to address the identified needs.
- Fluid Replacement: Administer oral or IV fluids as ordered, monitoring fluid intake and output closely to ensure adequate replacement.
- Electrolyte Correction: Administer electrolytes intravenously or orally as indicated by laboratory values.
- Monitor Hemodynamic Status: Closely monitor vital signs, particularly heart rate and blood pressure, to assess the patient’s hemodynamic response to fluid replacement therapy.
- Provide Comfort Measures: Offer frequent oral care, provide cool compresses, and assist with positioning to promote comfort.
- Educate Patient and Family: Explain the importance of fluid intake, signs and symptoms of dehydration, and potential complications.
Evaluation
The nursing care plan is not static; it is continuously evaluated to determine its effectiveness in achieving desired outcomes. The nurse will assess the patient’s progress, reassess vital signs, monitor fluid intake and output, and evaluate electrolyte levels to gauge the effectiveness of interventions.
Tips and Expert Advice
Here are some additional tips and expert advice for managing fluid volume deficit:
- Identify high-risk patients: Patients with conditions such as gastrointestinal disorders, elderly individuals, infants, and those with impaired cognitive function are more susceptible to dehydration.
- Promote oral hydration: Encourage frequent sips of water or electrolyte solutions throughout the day to prevent dehydration.
- Limit caffeine and alcohol: These substances can have diuretic effects and worsen dehydration.
- Educate patients about dehydration: Promote awareness of the importance of staying hydrated, particularly during hot weather or physical exertion.
- Monitor IV fluids carefully: Closely monitor IV fluid rates and monitor for signs of fluid overload, such as edema and shortness of breath.
Remember, early intervention is key to preventing serious complications associated with fluid volume deficit. It’s crucial to assess patients thoroughly, communicate effectively with the healthcare team, and provide personalized care tailored to individual needs.
Frequently Asked Questions
Here are some frequently asked questions about fluid volume deficit:
Q: What are some common causes of dehydration in children?
A: Children are more susceptible to dehydration because they have a higher percentage of body water compared to adults. Common causes of dehydration in children include diarrhea, vomiting, fever, and insufficient fluid intake.
Q: How can I prevent dehydration?
A: Staying adequately hydrated is essential for overall health. Drinking plenty of water, especially during hot weather or physical activity, is a crucial preventive measure.
Q: What are some signs of dehydration in infants?
A: Signs of dehydration in infants can include lethargy, sunken eyes, dry mouth, fewer wet diapers, and a rapid heartbeat. Seek medical attention immediately if you suspect your infant is dehydrated.
Q: Can dehydration lead to kidney stones?
A: Dehydration can contribute to the formation of kidney stones by increasing the concentration of minerals in the urine, making it more likely for crystals to form.
Q: How long does it take for the body to recover from dehydration?
A: The time it takes to recover from dehydration depends on the severity of dehydration and the individual’s overall health. Mild dehydration can be resolved by drinking fluids within a few hours. However, severe dehydration may require medical intervention and can take longer to recover.
Fluid Volume Deficit Nursing Care Plan
Conclusion
Fluid volume deficit, or dehydration, is a prevalent condition that can have significant health consequences. By understanding the causes, symptoms, and nursing interventions, nurses play a vital role in providing safe and effective care for patients experiencing fluid volume deficit. A comprehensive nursing care plan that emphasizes accurate assessment, appropriate fluid replacement, and ongoing monitoring can help restore fluid balance and prevent complications. Remember, early detection and intervention are crucial in managing fluid volume deficit and improving patient outcomes.
Are you interested in learning more about fluid volume deficit and how it impacts patients? Share your thoughts and questions in the comments below.






