Imagine a scene: a bustling hospital ward, filled with the hum of machines and a constant stream of healthcare professionals. Nurses, with their practiced hands and compassionate hearts, are constantly navigating the complex world of patient care. But amidst this flurry of activity, a lurking danger lurks – infection. It’s a threat that can turn a routine recovery into a perilous battle. But how can nurses ensure patient safety and fight against this invisible enemy? The answer lies in a powerful tool – a nursing care plan for risk for infection. This comprehensive guide is not just a document but a roadmap for preventing infection and safeguarding patient well-being, which is why it’s a vital document for every nurse.

Image: ryleighyouthmorales.blogspot.com
A nursing care plan for risk for infection is a detailed plan of care meticulously crafted to identify, assess, and minimize the risk of infection in patients. Think of it as a safety net, carefully designed to protect patients from potentially devastating complications. This plan is not a rigid template but a flexible framework that adapts to each patient’s unique situation, taking into account their individual needs, medical history, and current environment.
Understanding the Importance of a Nursing Care Plan for Risk for Infection
Infection control is a cornerstone of safe and effective patient care. It’s not just about preventing the spread of disease; it’s about protecting vulnerable individuals from potentially life-threatening complications. The reality is that infections can significantly impact a patient’s recovery, increase their length of stay in the hospital, and lead to additional medical interventions, all of which strain resources and can even be fatal.
A nursing care plan for risk for infection acts as a crucial weapon in the fight against this threat.
Here’s a breakdown of its key components:
1. Assessment:
-
Identifying Risk Factors: The journey starts with a meticulous assessment of the patient’s risk factors. Nurses delve into the patient’s medical history, current condition, and any factors that might increase their susceptibility to infection. These factors can range from chronic illnesses like diabetes or HIV to invasive procedures like surgery or the use of catheters.
-
Clinical Evaluation: The assessment includes a thorough physical examination, evaluating factors like skin integrity, respiratory status, and any signs of infection.
-
Environmental Evaluation: The environment also plays a significant role in infection risk. Nurses carefully analyze the patient’s surroundings, considering factors like the cleanliness of their room, the effectiveness of hand hygiene practices, and the potential for cross-contamination.
-
Monitoring and Observation: Nurses closely monitor patients for any signs of infection. Fever, redness, swelling, or changes in vital signs – these are red flags that demand immediate attention and intervention.
2. Planning:
-
Defining Goals: Once the assessment is complete, nurses collaborate with the medical team to establish specific, measurable, achievable, relevant, and time-bound (SMART) goals for infection prevention.
-
Developing Interventions: This is where the plan takes shape. Each goal is linked to specific interventions designed to reduce the risk of infection. These interventions can include a wide range of measures, from basic hand hygiene and isolation precautions to more complex treatments like antibiotic therapy or surgical intervention.
3. Implementation:
-
Putting the Plan into Action: The planning phase sets the stage for action. Implementing the interventions outlined in the plan is crucial. This involves diligently adhering to the prescribed protocols and procedures while providing the highest level of care to ensure patient safety.
-
Continuous Evaluation: The work doesn’t end once the plan is implemented. Nurses continuously monitor the patient’s progress, noting any changes in their condition or any signs of infection. Based on this ongoing evaluation, they adjust the plan as needed, making it a dynamic process that adapts to evolving needs.
-
Communication and Collaboration: Effective communication is paramount. Nurses remain in constant communication with the medical team, updating them on the patient’s condition and any concerns they may have about infection risk. This collaborative approach ensures that all members of the healthcare team are on the same page and working together to achieve the best possible outcome for the patient.
4. Evaluation:
-
Assessing Progress: Regular evaluation is essential to determine the effectiveness of the plan. Nurses assess the patient’s response to interventions, measuring the plan’s impact on reducing infection risk.
-
Modifications: If the plan isn’t achieving the desired outcomes, nurses work with the medical team to modify it, adjusting interventions or incorporating new strategies tailored to the patient’s evolving needs.
The Power of the PDF
Now that we understand the foundational principles of infection control, let’s dive into the specifics of a nursing care plan for risk of infection. This comprehensive plan is often documented in a PDF format. Think of it as a detailed roadmap that nurses can utilize to guide their care and ensure patient safety.
Key Elements of a Nursing Care Plan for Risk for Infection PDF:
-
Patient Profile: This section details the patient’s essential information: name, age, medical history, current condition, medications, and any factors that might increase their risk of infection.
-
Assessment Data: This is the heart of the document. Nurses compile data from their assessment, outlining the identified risk factors, any signs or symptoms of infection, and any environmental factors contributing to risk.
-
Goals: Each identified risk factor or concern is linked to a specific, measurable goal designed to reduce the risk of infection.
-
Interventions: Detailed interventions are listed alongside each goal. These interventions include specific actions that nurses will implement to achieve the goals.
-
Evaluation: The document outlines how nurses will evaluate the effectiveness of interventions and track the patient’s progress.
-
Documentation: The document provides a space for nurses to document their observations, interventions, and any changes to the plan over time.
-
References: The document may include links to relevant resources or guidelines for additional guidance on infection control measures.
Real-World Applications of Nursing Care Plans for Risk of Infection
Let’s explore some practical examples to illustrate the real-world significance of this powerful tool:
-
Surgery: A patient undergoing surgery is at a heightened risk for infection. A nursing care plan would outline interventions such as sterile technique during procedures, meticulous wound care, and medication administration to manage potential complications.
-
Immunocompromised Individuals: Patients with weakened immune systems are particularly vulnerable to infections. The nursing care plan would focus on stringent infection prevention measures like isolation precautions, hand hygiene, and careful monitoring for any signs of infection.
-
Long-term Care Facilities: Residents in long-term care facilities are often prone to infections due to age, underlying medical conditions, and their dependence on caregivers. The nursing care plan would emphasize preventative measures like regular hand hygiene, prompt wound care, and thorough environmental cleaning.
-
Home Health: Patients receiving care in their homes also benefit from a nursing care plan for risk of infection. The plan would address specific environmental hazards, educate family members on infection prevention strategies, and provide guidance for managing potential complications.
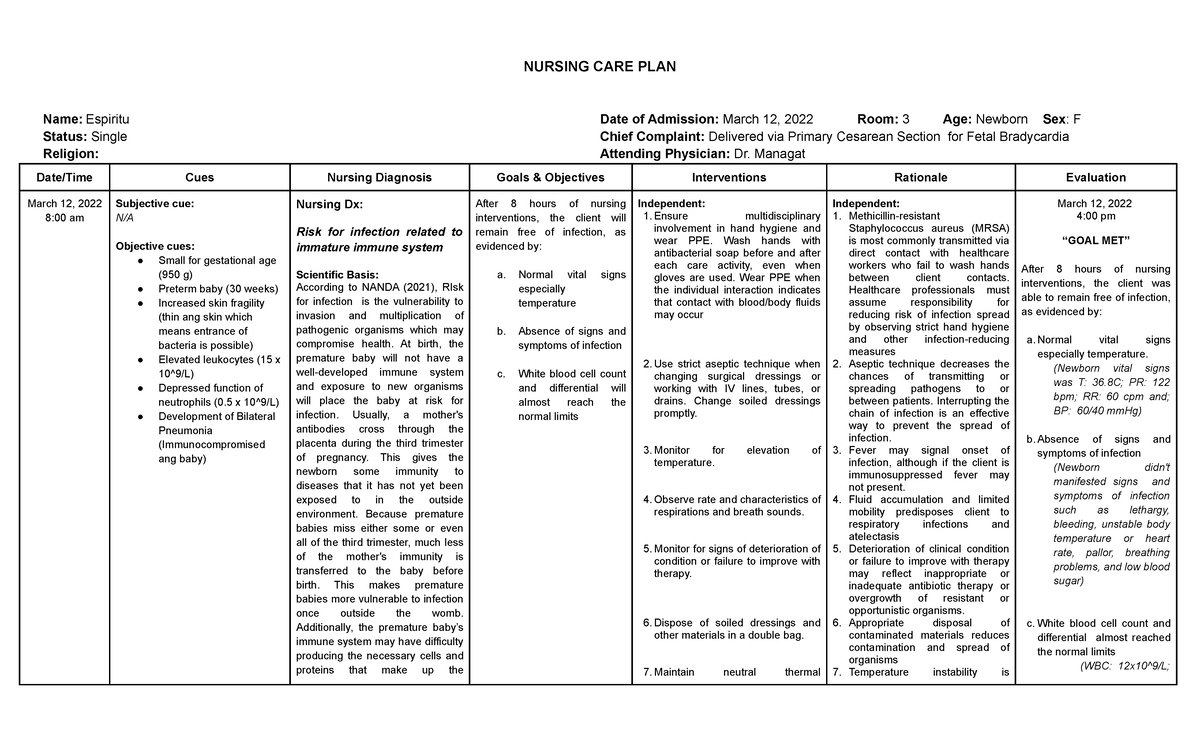
Image: www.vrogue.co
Expert Insights for Nurses
Effective infection control is a collaborative effort, requiring the expertise of nurses, doctors, other healthcare professionals, and the patient themselves. Here’s what the experts emphasize:
-
Hand Hygiene: This is the cornerstone of infection prevention. Washing hands thoroughly and frequently, particularly before and after patient contact, is a vital habit that can save lives.
-
Isolation Precautions: When dealing with patients with contagious infections, strict isolation precautions are essential. This includes wearing protective gear, limiting contact with other patients, and using dedicated equipment.
-
Environmental Control: Maintaining a clean and disinfected environment is crucial. Nurses should ensure that patient rooms are regularly cleaned, surfaces are disinfected, and contaminated materials are disposed of properly.
-
Patient Education: Empowering patients to participate in their own care is crucial. Nurses should educate patients and their families about infection prevention practices, emphasizing the importance of hand hygiene, proper personal hygiene, and preventing the spread of germs.
Nursing Care Plan For Risk For Infection Pdf
Harnessing the Power of the Nursing Care Plan for Risk for Infection
The nursing care plan for risk of infection is a valuable tool that empowers nurses to provide safe, effective, and compassionate care. It’s an integral part of a comprehensive infection control strategy, guiding nurses through the vital process of identifying, assessing, and minimizing infection risks.
By embracing this plan, nurses can play a proactive role in protecting their patients from the threat of infection, fostering safe and healthy environments. As you explore this powerful tool, remember that you’re not just using a document; you’re harnessing the power of knowledge, expertise, and compassion to make a real difference in the lives of those entrusted to your care.
A Call to Action:
Share your experiences with nursing care plans for risk of infection! Do you have any tips for creating effective plans or overcoming challenges related to infection control? Let’s continue the conversation and learn from one another in the comments section below.






