Imagine a parched desert, where the sun beats down relentlessly and life struggles to thrive. That’s what a fluid volume deficit resembles in the human body. It’s a critical condition where the body lacks sufficient fluids to function properly, leading to a cascade of complications. This is where the expertise of nurses shines, as they act as vigilant guardians, recognizing the signs of dehydration and intervening with timely and effective care.
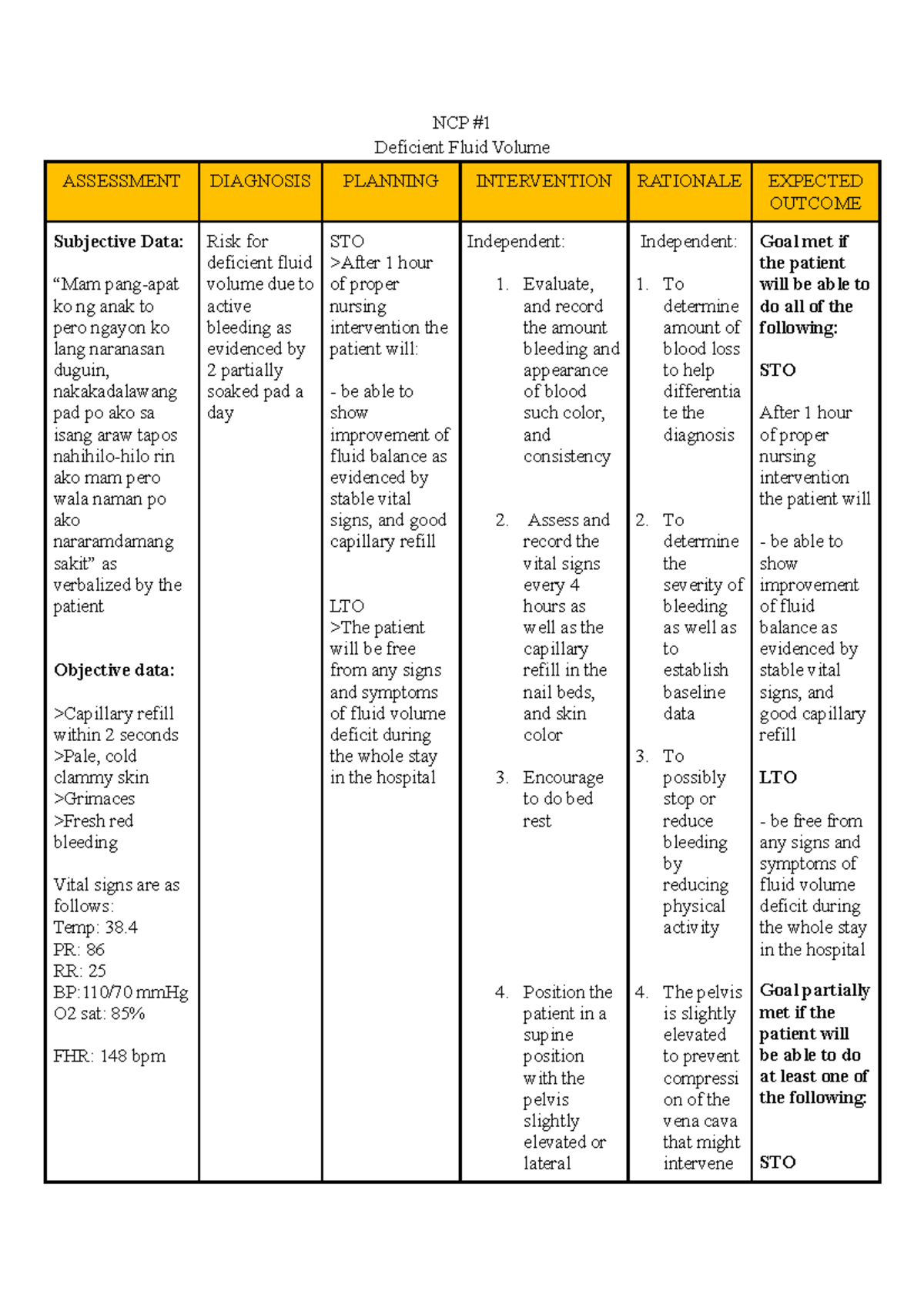
Image: www.vrogue.co
Fluid volume deficit, sometimes referred to as hypovolemia, is a multifaceted nursing diagnosis that requires a nuanced understanding. This article will unravel the complexities of this condition, delving into its causes, symptoms, and crucial nursing interventions, shedding light on how nurses play a pivotal role in restoring fluid balance and safeguarding patient well-being. Understanding this complex diagnosis can empower healthcare professionals to provide better care for those suffering from fluid imbalance and potentially life-threatening complications.
Deciphering the Diagnosis: Causes and Risk Factors
Fluid volume deficit arises from a delicate imbalance between fluid intake and output. The body constantly strives to maintain a delicate equilibrium, but various factors can disrupt this harmony, leading to dehydration. One of the most common causes is inadequate fluid intake, which can be exacerbated by factors such as:
- Limited Access to Fluids: Elderly individuals, particularly those with cognitive impairment, may struggle to access water independently.
- Reduced Thirst Sensation: Conditions like diabetes, kidney disease, and certain medications can decrease the body’s ability to perceive thirst.
- Dietary Restrictions: Individuals with dietary restrictions, such as those following a low-sodium diet, may inadvertently restrict fluid intake.
Another significant contributor to fluid volume deficit is excessive fluid loss. This can stem from various sources, including:
- Excessive Sweating: Vigorous exercise, hot environments, and fever can trigger excessive sweating, leading to fluid depletion.
- Gastrointestinal Losses: Vomiting, diarrhea, and gastrointestinal bleeding can lead to significant fluid loss, particularly in younger children and older adults.
- Renal Losses: Conditions like kidney disease can impair the kidney’s ability to conserve fluids, leading to excessive urine production.
- Wound Drainage: Significant fluid loss can occur through open wounds or surgical sites, especially after trauma or surgery.
Certain individuals are more susceptible to fluid volume deficit. Risk factors include:
- Infants and Children: They have a higher fluid turnover rate and are more vulnerable to dehydration because their bodies are smaller.
- Older Adults: As we age, our thirst sensation can diminish, and our bodies are less efficient at conserving fluids.
- Individuals with Chronic Illnesses: Conditions like diabetes, heart failure, and kidney disease can increase the risk of fluid imbalances.
- Athletes: Intense physical activity can lead to significant fluid loss through sweating, particularly in hot weather.
Unveiling the Signs: Recognizing Fluid Volume Deficit
Early detection is paramount in managing fluid volume deficit. Nurses play a crucial role in recognizing subtle signs that may signal an impending fluid imbalance. These symptoms range from mild to severe and may vary depending on the individual’s overall health and the severity of the fluid loss.
Early warning signs may include:
- Dry Mouth: Dryness in the mouth can be an early indicator that the body is lacking sufficient fluids.
- Decreased Urine Output: Reduced urine production is a crucial sign that the body is struggling to maintain adequate fluid levels.
- Headache: Dehydration can cause headaches, particularly in individuals who are susceptible to migraines.
- Lightheadedness: Low blood volume, a hallmark of fluid deficit, can cause dizziness and lightheadedness.
- Increased Fatigue: The body requires adequate fluids to function optimally, and dehydration can lead to exhaustion and fatigue.
As the fluid deficit worsens, more pronounced signs emerge:
- Tachycardia (Increased Heart Rate): The heart compensates for decreased blood volume by beating faster to maintain adequate oxygen delivery.
- Hypotension (Low Blood Pressure): Reduced blood volume can lead to a drop in blood pressure, which is a significant sign of dehydration.
- Sunken Eyes: Loss of fluids can cause the eyes to appear sunken, reflecting the body’s attempt to conserve fluids.
- Dry Skin: Dehydrated skin can become dry, lose its elasticity, and appear flaky.
- Rapid Breathing: The body may increase respiration rate to compensate for decreased oxygen levels due to low blood volume.
- Alterations in Consciousness: In severe cases, dehydration can lead to confusion, disorientation, or even loss of consciousness.
A Nurse’s Role: Restoring Fluid Balance
Nurses are the cornerstone of patient care, constantly vigilant to identify and address fluid imbalances. They utilize a multifaceted approach to manage fluid volume deficit, incorporating a combination of assessments, interventions, and meticulous monitoring.
Image: www.coursehero.com
Assessment and Monitoring
The first step in managing fluid volume deficit is a comprehensive assessment of the patient’s condition. Nurses meticulously assess:
- Vital Signs: Monitoring body temperature, heart rate, blood pressure, and respiratory rate provides valuable insights into the severity of dehydration.
- Fluid Intake and Output: Tracking the amount of fluids consumed and eliminated (urine, stool, vomit) helps gauge fluid balance.
- Skin Turgor: Assessing skin elasticity gives an indication of hydration levels. Gently pinch the skin on the back of the hand or forehead, and observe how quickly it returns to its normal shape.
- Mucous Membranes: Observing the moisture and color of the mucous membranes (inside the mouth and nose) provides clues about hydration status.
- Mental Status: Evaluating the patient’s level of consciousness, alertness, and orientation to time and place is critical, especially in cases of severe dehydration.
Interventions
Depending on the severity of the fluid deficit, nurses implement interventions to restore fluid balance. Common interventions include:
- Oral Rehydration: Encouraging the patient to drink fluids is the first line of defense. Water is the best choice for most individuals, but electrolyte-rich beverages like sports drinks or oral rehydration solutions (ORS) can be more effective in cases of significant fluid loss.
- Intravenous (IV) Fluid Therapy: For severe fluid deficit, intravenous fluids are administered to rapidly replenish fluids and electrolytes. Nurses carefully monitor the patient’s response to IV therapy, adjusting the infusion rate and type of fluids as needed.
- Medication Administration: Anti-emetics to control vomiting and antidiarrheals to manage diarrhea can reduce fluid loss in specific cases.
- Monitoring for Complications: Nurses continuously monitor for complications like electrolyte imbalances, kidney dysfunction, and shock, and promptly notify the healthcare provider if they arise.
Patient Education
Nurses play a crucial role in educating patients and their caregivers about fluid volume deficit. This education empowers them to prevent future episodes of dehydration. Key aspects of patient education include:
- Importance of Maintaining Adequate Hydration: Emphasize the crucial role of staying hydrated and the risks associated with fluid deficit.
- Identifying Risk Factors: Educate patients about individual risk factors for dehydration, such as chronic illnesses, medications, and lifestyle factors.
- Recognizing Warning Signs: Teach patients and their family members to identify early signs of fluid volume deficit and encourage them to seek medical attention promptly.
- Fluid Intake Recommendations: Provide guidance on the recommended daily fluid intake based on age, activity level, and climate.
Navigating the Future: Trends and Advancements
The field of fluid volume deficit management is constantly evolving. Advancements in technology and research are leading to new strategies and interventions. For instance, the use of point-of-care testing devices allows nurses to measure electrolyte levels quickly and accurately, facilitating more precise fluid replacement therapy.
Furthermore, research is exploring the role of innovative interventions, such as hydration interventions targeted at specific populations, like older adults and those with chronic illnesses. The focus is on personalized approaches that consider individual risk factors and needs, ensuring effective prevention and management of fluid volume deficit.
Nursing Diagnosis Of Fluid Volume Deficit
Conclusion: Empowering Nurses, Saving Lives
Fluid volume deficit is a silent threat that can quickly escalate into a life-threatening condition. Nurses are the frontline champions in recognizing this condition, implementing appropriate interventions, and guiding patients through the journey back to fluid balance. By understanding the nuances of this nursing diagnosis, nurses can empower themselves and their patients to prevent and manage dehydration effectively, ultimately ensuring optimal health and well-being. Remember, every drop of fluid counts, and nurses are the guardians of those precious drops. Let us all contribute to a world where dehydration becomes a distant memory, replaced by a culture of proactive hydration and mindful fluid management.






